-
Hey, guest user. Hope you're enjoying NeoGAF! Have you considered registering for an account? Come join us and add your take to the daily discourse.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
I am vaccinated. But sending kids to school unprotected is a really bad idea with Delta. I hope the people in charge can live with the consequences of their recklessness.Breathe into a paper bag and stay home, work safe. The rest of us are going to go on about our lives.
100% will get it if unprotected according to Christian Drosten (world-renowned virologist, discoverer of SARS and MERS, developer of first Covid19-Test). Stats are from UK.Which % of kids actually gets it though?
(if stats are from India, I'd be a bit skeptical about official figures)
Last edited:
D
Deleted member 17706
Unconfirmed Member
Japan especially puzzles me. They still want to hold the Olympics so why didn't they acquire as much vaccines as they could get a hold of? Or perhaps they did try and they just can't get any? I haven't been following it closely and I want to know what their deal is.
There are a variety of factors.
Vaccine hesitancy in general is pretty high in Japan and has been growing over the last couple of decades. Combine this with the fact that the COVID vaccines are mostly new technology and developed by foreign-owned companies and the sense of mistrust increases. If it were a domestically developed vaccine, social confidence would be much higher, but domestic pharmaceutical companies have not made vaccine development a priority for many different reasons, and the government has not incentivized investment in this area either.
Safety is also a huge deal for most Japanese people. While other countries are enlisting volunteers that have zero medical background to administer injections, that will likely never fly in Japan. The population basically will only trust doctors and nurses, and there was criticism against officials for even suggesting that pharmacy employees might be given emergency authorization administer shots. Even before the lack of vaccine doses, there is a severe lack of people qualified to give the shots in the country.
I think that by far the biggest reason, however, is that COVID-19 just hasn't been very bad in Japan compared to a lot of the world. 2020 saw lower total mortality than 2019. The COVID-19 deaths recorded in 2020 were just about the same as the deaths to influenza in 2019 and influenza was basically eliminated (or replaced) in 2020. Without a massive death toll, it's hard to get people to rush towards getting a vaccination they are not confident in and there is growing sentiment that the government is only pushing them (in combination with their state of emergency declarations) so that they can improve their numbers leading into the Olympics, which something like 70% of the country doesn't even want to go forward in the first place.
In short, a lack of urgency and trust.
Last edited by a moderator:
DeepBreath87
Banned
I sent my kids to school all year. We’re living just fine. Don’t you worry, big guy.I am vaccinated. But sending kids to school unprotected is a really bad idea with Delta. I hope the people in charge can live with the consequences of their recklessness.
watThe government said they did, but you can check airport sites and still see them coming in every day.
Either the government are lying, or the airports are doing it without their knowledge.
Birdo
Banned
The government said they did, but you can check airport sites and still see them coming in every day.
Either the government are lying, or the airports are doing it without their knowledge.
Raven117
Member
And if data shows that there is a high hospitalization/death rate among children in the west, then policy can be adjusted.I am vaccinated. But sending kids to school unprotected is a really bad idea with Delta. I hope the people in charge can live with the consequences of their recklessness.
There will always be the “next scary thing.”
Raven117
Member
When responding to hyperbole (disguised as “concern”) then yes.Do we have to go with hyperbole every single time?
It would nice to have an actual discussion.
Rentahamster
Rodent Whores
No, you actually don't have to do that because that does not steer the conversation towards grounded reality and the truth.When responding to hyperbole (disguised as “concern”) then yes.
pr0cs
Member
Those numbers are pretty hard to find, probably by designdeath rate among children in the west
Airola
Member
I've seen nothing to suggest that any variants are dodging the vaccines.
No, it isn’t. 40% more transmissible. Zero evidence to suggest it’s more serious or can avoid vaccines.
I don't know about zero evidence.
In Finland we had sort of an epidemic in a group of hospitals where 80 people got infected and the majority were vaccinated at least once.
And 11% of hospital workers who had been vaccinated twice and had special masks had been infected too.
It was the Indian variant.
I have no idea how serious that is or if there's some other explanation than "vaccine avoidance" or whatever for the virus, but this still happened and it has been officially reported by the hospitals.
BadBurger
Is 'That Pure Potato'
I am vaccinated. But sending kids to school unprotected is a really bad idea with Delta. I hope the people in charge can live with the consequences of their recklessness.
Yep.

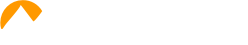
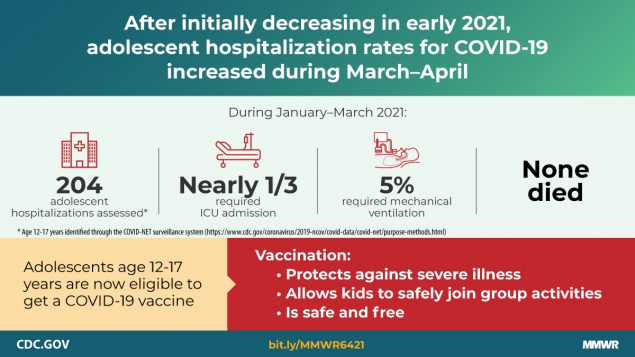
COVID-19 still poses severe risk to unvaccinated teens: CDC
Nearly a third of teens ages 12-17 with COVID-19 ended up in the intensive care unit, with 5% ultimately being placed on ventilators.
terintamel
Member
For my state in the US here are our reported stats for 0-19 year olds since the pandemic began.
~115,106 total positive cases
~13 deaths
~0.011% mortality rate
They do not report hospitalization rates. So based on those numbers to me it looks like the overwhelming majority of children in school will be just fine without a vaccine.
For comparission the CDC 2017 general mortality rate per 100k for the 0-19 age group is 0.75%
Also in my state 91.9% of all reported Covid deaths are in the 60+ age group.
~115,106 total positive cases
~13 deaths
~0.011% mortality rate
They do not report hospitalization rates. So based on those numbers to me it looks like the overwhelming majority of children in school will be just fine without a vaccine.
For comparission the CDC 2017 general mortality rate per 100k for the 0-19 age group is 0.75%
Also in my state 91.9% of all reported Covid deaths are in the 60+ age group.
Last edited:
DeepBreath87
Banned
Ok. That quote is not accurate. Even from the article. This is what it actually says:Yep.

COVID-19 still poses severe risk to unvaccinated teens: CDC
Nearly a third of teens ages 12-17 with COVID-19 ended up in the intensive care unit, with 5% ultimately being placed on ventilators.abcnews.go.com
Your quote says something completely different. See if you can spot it.Nearly a third of teens ages 12-17 hospitalized with COVID-19 ended up in the intensive care unit, with 5% ultimately being placed on ventilators.
Nowhere in that article does it list the actual number of hospitalized teens. This is crucial in understanding the nature of the risk posed to this age group. Also, it says this:
Most of the teens who were hospitalized with COVID-19, approximately 70%, had at least one underlying medical condition
Last edited:
BadBurger
Is 'That Pure Potato'
Ok. That quote is not accurate. Even from the article. This is what it actually says:
Your quote says something completely different. See if you can spot it.
Nowhere in that article does it list the actual number of hospitalized teens. This is crucial in understanding the nature of the risk posed to this age group. Also, it says this:
nope I’m good.
I don't mess around with anti-science people.
Last edited:
fear pornYep.

COVID-19 still poses severe risk to unvaccinated teens: CDC
Nearly a third of teens ages 12-17 with COVID-19 ended up in the intensive care unit, with 5% ultimately being placed on ventilators.abcnews.go.com
covid19 is not a severe risk to teens. just look at the data
DeepBreath87
Banned
Well try again. Because you’re not good. Your quote says:nope I’m good.
Nearly a third of teens age 12-17 with covid 19 ended up in intensive care…
The article says:
Nearly a third of teens ages 12-17 hospitalized with COVID-19 ended up in the intensive care unit, with 5% ultimately being placed on ventilators
Let me know if you need help figuring out why those two quotes mean different things. I gave you a hint…
xrnzaaas
Member
If the parents and the grandparents already had covid and/or got vaccinated, then you really shouldn't exaggerate with the fears. Kids will have to go back to school eventually and yes they will get sick from other kids like they have before the pandemic.100% will get it if unprotected according to Christian Drosten (world-renowned virologist, discoverer of SARS and MERS, developer of first Covid19-Test). Stats are from UK.
Rentahamster
Rodent Whores
Here is the research that this article is based on:Nowhere in that article does it list the actual number of hospitalized teens. This is crucial in understanding the nature of the risk posed to this age group.
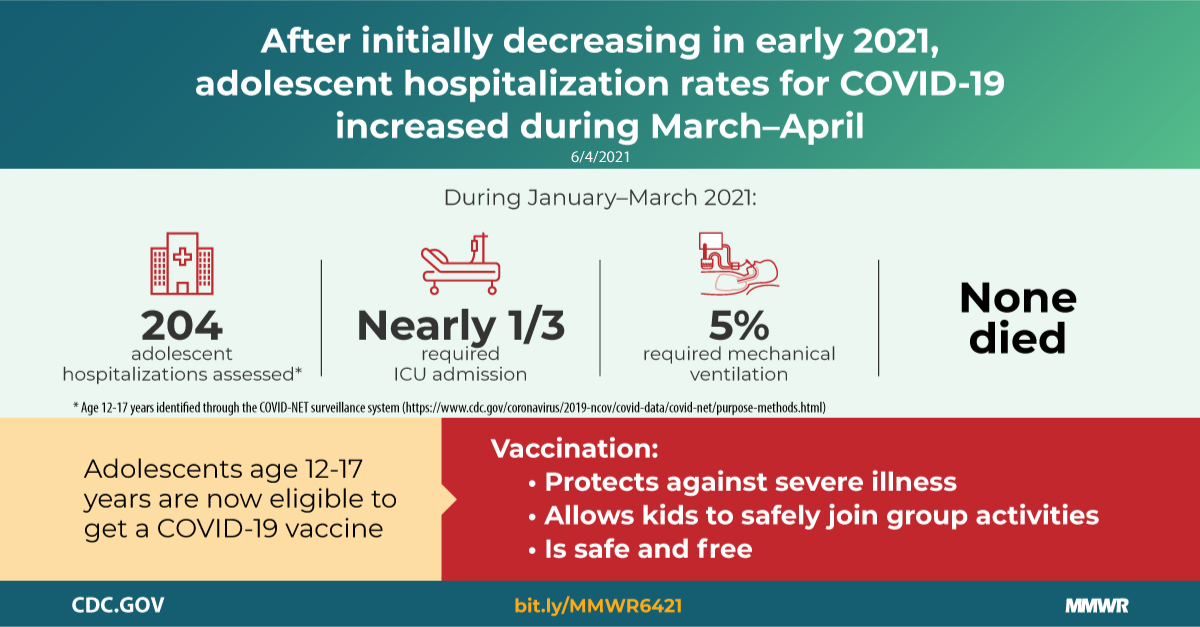
Hospitalization of Adolescents Aged 12–17 Years with ...
COVID-19 adolescent hospitalization rates peaked at 2.1 ...
Summary
What is already known about this topic?Most COVID-19–associated hospitalizations occur in adults, but severe disease occurs in all age groups, including adolescents aged 12–17 years.
What is added by this report?
COVID-19 adolescent hospitalization rates from COVID-NET peaked at 2.1 per 100,000 in early January 2021, declined to 0.6 in mid-March, and rose to 1.3 in April. Among hospitalized adolescents, nearly one third required intensive care unit admission, and 5% required invasive mechanical ventilation; no associated deaths occurred.
What are the implications for public health practice?
Recent increased hospitalization rates in spring 2021 and potential for severe disease reinforce the importance of continued COVID-19 prevention measures, including vaccination and correct and consistent mask wearing among persons not fully vaccinated or when required.
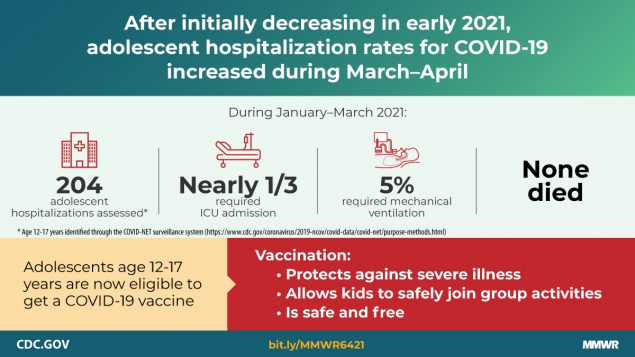
Cumulative COVID-19–associated hospitalization rates during October 1, 2020–April 24, 2021, were 2.5–3.0 times higher than were influenza-associated hospitalization rates from three recent influenza seasons (2017–18, 2018–19, and 2019–20) obtained from the Influenza Hospitalization Surveillance Network (FluSurv-NET). Recent increased COVID-19–associated hospitalization rates in March and April 2021 and the potential for severe disease in adolescents reinforce the importance of continued COVID-19 prevention measures, including vaccination and correct and consistent wearing of masks by persons not yet fully vaccinated or when required by laws, rules, or regulations.
COVID-NET data indicate that COVID-19–associated hospitalization rates were lower in adolescents aged 12–17 years compared with those in adults but exceeded those among children aged 5–11 years during March 1, 2020–April 24, 2021. Moreover, COVID-19–associated hospitalization rates among adolescents increased during March–April 2021, and nearly one third of 204 recently hospitalized adolescents required ICU admission. Rates of COVID-19–associated hospitalization among adolescents also exceeded historical rates of seasonal influenza-associated hospitalization during comparable periods. Recent increased hospitalization rates and the potential for severe disease reinforce the importance of continued COVID-19 prevention measures among adolescents, including vaccination and correct and consistent wearing of masks.
Population-based COVID-19–associated hospitalization rates among adolescents were lower than were those in adults, a finding consistent with studies showing that illness is generally milder in children than in adults (6). Nevertheless, severe disease does occur, including that requiring ICU admission and invasive mechanical ventilation. Most (70.6%) adolescents in this study whose primary reason for hospitalization was COVID-19–associated illness had at least one underlying medical condition, which is lower than the percentage of hospitalized adults with an underlying medical condition (92%) (7). Nearly 30% of these adolescents had no reported underlying medical condition, indicating that healthy adolescents are also at risk for severe COVID-19–associated disease. In addition, approximately two thirds of adolescents hospitalized with COVID-19 were Hispanic or non-Hispanic Black persons, consistent with studies showing an increased incidence of COVID-19 among racial and ethnic minority populations and signifying an urgent need to ensure equitable access to vaccines for these groups (8). Vaccination is effective in preventing hospitalization among adults (9); similarly, widespread vaccination of adolescents will likely reduce COVID-19–associated hospitalizations, and potential sequelae from COVID-19 in adolescents, including multisystem inflammatory syndrome in children (MIS-C), a rare but serious complication of COVID-19 (10).
During a comparable period, adolescent hospitalization rates associated with COVID-19 exceeded those for seasonal influenza, another respiratory virus that can cause hospitalization and death in adolescents and for which a vaccine is recommended in this age group.††† This widespread circulation of SARS-CoV-2 occurred despite containment measures such as school closures, wearing masks, and physical distancing, none of which had been enacted during the historical influenza seasons. Without these containment measures, the rates of COVID-19–associated hospitalization might have been substantially higher.
The findings in this report are subject to at least five limitations. First, the primary reason for hospital admission was not always clear, and some (45.7%) adolescents who met the COVID-NET case definition were hospitalized for reasons that might not have been primarily related to COVID-19, despite a positive SARS-CoV-2 laboratory test result; these hospitalizations were included in rate calculations. Thus, rates of hospitalizations for COVID-19 might be overestimated. Second, laboratory confirmation depends on clinician-ordered testing and hospital testing policies for SARS-CoV-2 (COVID-NET) and influenza (FluSurv-NET); consequently, hospitalization rates might also be underestimated. Given more widespread testing for SARS-CoV-2 compared with influenza, the lack of adjustment for testing practices likely disproportionately affects influenza rates compared with COVID-19 rates. Third, adolescents hospitalized with MIS-C might not be identified if testing occurred >14 days before admission, potentially leading to an underestimate of severe COVID-19–associated disease. Fourth, the Pfizer-BioNTech COVID-19 vaccine had been approved for and administered to adolescents aged 16–17 years during this study period; therefore, rates of COVID-19–associated hospitalization in adolescents aged 16–17 years might differ from those in adolescents aged 12–15 years who were not previously eligible for vaccination, and could affect the overall hospitalization rate for all adolescents. Finally, hospitalization rates are preliminary and might change as additional data are reported.
Raven117
Member
Yup. Can’t generate fear porn if give out those numbers. While people on the thread just can’t seem to get over that covid is over in the US and society is getting back to normal. It’s not by accident that the focus is on kids (because they are the only major group not vaccinated…. The only group where you can still play the fear porn game because all the major vaccines are effective against it).Those numbers are pretty hard to find, probably by design
And, if it poses a real risk to children, then we change policy.
This fear porn at this stage is just sad and pathetic. Losers hold onto covid.
Last edited:
DeepBreath87
Banned
So 204 12-17 year olds hospitalized over 3 months in the whole country? This is a “severe risk”? I wonder how many hospitalization there were for people in that age group falling down the steps during the same period. Maybe steps pose a severe risk too to teenagers too.Here is the research that this article is based on:
Hospitalization of Adolescents Aged 12–17 Years with ...
COVID-19 adolescent hospitalization rates peaked at 2.1 ...www.cdc.gov
Summary
What is already known about this topic?
Most COVID-19–associated hospitalizations occur in adults, but severe disease occurs in all age groups, including adolescents aged 12–17 years.
What is added by this report?
COVID-19 adolescent hospitalization rates from COVID-NET peaked at 2.1 per 100,000 in early January 2021, declined to 0.6 in mid-March, and rose to 1.3 in April. Among hospitalized adolescents, nearly one third required intensive care unit admission, and 5% required invasive mechanical ventilation; no associated deaths occurred.
What are the implications for public health practice?
Recent increased hospitalization rates in spring 2021 and potential for severe disease reinforce the importance of continued COVID-19 prevention measures, including vaccination and correct and consistent mask wearing among persons not fully vaccinated or when required.
Cumulative COVID-19–associated hospitalization rates during October 1, 2020–April 24, 2021, were 2.5–3.0 times higher than were influenza-associated hospitalization rates from three recent influenza seasons (2017–18, 2018–19, and 2019–20) obtained from the Influenza Hospitalization Surveillance Network (FluSurv-NET). Recent increased COVID-19–associated hospitalization rates in March and April 2021 and the potential for severe disease in adolescents reinforce the importance of continued COVID-19 prevention measures, including vaccination and correct and consistent wearing of masks by persons not yet fully vaccinated or when required by laws, rules, or regulations.
COVID-NET data indicate that COVID-19–associated hospitalization rates were lower in adolescents aged 12–17 years compared with those in adults but exceeded those among children aged 5–11 years during March 1, 2020–April 24, 2021. Moreover, COVID-19–associated hospitalization rates among adolescents increased during March–April 2021, and nearly one third of 204 recently hospitalized adolescents required ICU admission. Rates of COVID-19–associated hospitalization among adolescents also exceeded historical rates of seasonal influenza-associated hospitalization during comparable periods. Recent increased hospitalization rates and the potential for severe disease reinforce the importance of continued COVID-19 prevention measures among adolescents, including vaccination and correct and consistent wearing of masks.
Population-based COVID-19–associated hospitalization rates among adolescents were lower than were those in adults, a finding consistent with studies showing that illness is generally milder in children than in adults (6). Nevertheless, severe disease does occur, including that requiring ICU admission and invasive mechanical ventilation. Most (70.6%) adolescents in this study whose primary reason for hospitalization was COVID-19–associated illness had at least one underlying medical condition, which is lower than the percentage of hospitalized adults with an underlying medical condition (92%) (7). Nearly 30% of these adolescents had no reported underlying medical condition, indicating that healthy adolescents are also at risk for severe COVID-19–associated disease. In addition, approximately two thirds of adolescents hospitalized with COVID-19 were Hispanic or non-Hispanic Black persons, consistent with studies showing an increased incidence of COVID-19 among racial and ethnic minority populations and signifying an urgent need to ensure equitable access to vaccines for these groups (8). Vaccination is effective in preventing hospitalization among adults (9); similarly, widespread vaccination of adolescents will likely reduce COVID-19–associated hospitalizations, and potential sequelae from COVID-19 in adolescents, including multisystem inflammatory syndrome in children (MIS-C), a rare but serious complication of COVID-19 (10).
During a comparable period, adolescent hospitalization rates associated with COVID-19 exceeded those for seasonal influenza, another respiratory virus that can cause hospitalization and death in adolescents and for which a vaccine is recommended in this age group.††† This widespread circulation of SARS-CoV-2 occurred despite containment measures such as school closures, wearing masks, and physical distancing, none of which had been enacted during the historical influenza seasons. Without these containment measures, the rates of COVID-19–associated hospitalization might have been substantially higher.
The findings in this report are subject to at least five limitations. First, the primary reason for hospital admission was not always clear, and some (45.7%) adolescents who met the COVID-NET case definition were hospitalized for reasons that might not have been primarily related to COVID-19, despite a positive SARS-CoV-2 laboratory test result; these hospitalizations were included in rate calculations. Thus, rates of hospitalizations for COVID-19 might be overestimated. Second, laboratory confirmation depends on clinician-ordered testing and hospital testing policies for SARS-CoV-2 (COVID-NET) and influenza (FluSurv-NET); consequently, hospitalization rates might also be underestimated. Given more widespread testing for SARS-CoV-2 compared with influenza, the lack of adjustment for testing practices likely disproportionately affects influenza rates compared with COVID-19 rates. Third, adolescents hospitalized with MIS-C might not be identified if testing occurred >14 days before admission, potentially leading to an underestimate of severe COVID-19–associated disease. Fourth, the Pfizer-BioNTech COVID-19 vaccine had been approved for and administered to adolescents aged 16–17 years during this study period; therefore, rates of COVID-19–associated hospitalization in adolescents aged 16–17 years might differ from those in adolescents aged 12–15 years who were not previously eligible for vaccination, and could affect the overall hospitalization rate for all adolescents. Finally, hospitalization rates are preliminary and might change as additional data are reported.
That article is a case study in framing for effect. Panic porn.
Last edited:
Rentahamster
Rodent Whores
No. 204 is just the group that they studied. You can find the per capita rates here:So 204 12-17 year olds hospitalized over 3 months in the whole country? This is a “severe risk”? I wonder how many hospitalization there were for people in that age group falling down the steps during the same period. Maybe steps are a severe risk too.
FIGURE 1. Three-week moving average COVID-19–associated hospitalization rates* among children and adolescents aged <18 years, by age group — COVID-NET, 14 states,† March 1, 2020–April 24, 2021
Abbreviation: COVID-NET = Coronavirus Disease 2019–Associated Hospitalization Surveillance Network.
* Number of patients with laboratory-confirmed COVID-19–associated hospitalizations per 100,000 population.
† COVID-NET sites are in the following 14 states: California, Colorado, Connecticut, Georgia, Iowa, Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah.
FIGURE 2. Cumulative rates for COVID-19–associated hospitalizations* compared with influenza-associated hospitalizations† among adolescents aged 12–17 years, by surveillance week§ — COVID-NET¶ and FluSurv-NET,** 14 states,†† 2017–2021§§
Abbreviations: COVID-NET = Coronavirus Disease 2019–Associated Hospitalization Surveillance Network; FluSurv-NET = Influenza Hospitalization Surveillance Network.
* Number of patients with laboratory-confirmed COVID-19-associated hospitalizations per 100,000 population.
† Number of patients with laboratory-confirmed influenza-associated hospitalizations per 100,000 population.
§ Surveillance week is based on the epidemiologic week for disease reporting and lasts Sundays through Saturdays. MMWR week numbering is sequential beginning with 1 and incrementing with each week to a maximum of 52 or 53. The three influenza seasons had no surveillance week 53, so values from surveillance week 52 were imputed to surveillance week 53. https://wwwn.cdc.gov/nndss/document/MMWR_week_overview.pdf
¶ COVID-NET is a population-based surveillance system of laboratory-confirmed COVID-19–associated hospitalizations in 99 counties across 14 states. COVID-19–associated hospitalizations among residents in a predefined surveillance catchment area who received a positive test for SARS-CoV-2 (the virus that causes COVID-19) during hospitalization or ≤14 days before admission are included in surveillance.
** FluSurv-NET is a population-based surveillance system of laboratory-confirmed influenza-associated hospitalizations in 81 counties across 13 states (for the period included) and is conducted annually during October 1–April 30. Influenza-associated hospitalizations among residents in a predefined surveillance catchment area who received a positive test for influenza during hospitalization or ≤14 days before admission are included in surveillance.
†† COVID-NET and FluSurv-NET sites were in the following 14 states for the period shown: California, Colorado, Connecticut, Georgia, Iowa (COVID-NET only), Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah.
§§ Cumulative COVID-19–associated hospitalization rates among adolescents aged 12–17 years during October 1, 2020–April 24, 2021, were compared with influenza-associated hospitalization rates in the same age group during October 1–April 30 across three seasons (2017–18, 2018–19, and 2019–20) using data from FluSurv-NET.
DeepBreath87
Banned
So there were 204 hospitalization over 3 months in 14 states tracked by this service during the height of the pandemic. 204 hospitalizations. Out of millions of people in this age group, in these states. 140 or so who had underlying medical conditions as teenagers, meaning the don’t not represent the broader population of people in this age group. Again. This is not a severe risk to people in this age group.No. 204 is just the group that they studied. You can find the per capita rates here:
FIGURE 1. Three-week moving average COVID-19–associated hospitalization rates* among children and adolescents aged <18 years, by age group — COVID-NET, 14 states,† March 1, 2020–April 24, 2021
Abbreviation: COVID-NET = Coronavirus Disease 2019–Associated Hospitalization Surveillance Network.
* Number of patients with laboratory-confirmed COVID-19–associated hospitalizations per 100,000 population.
† COVID-NET sites are in the following 14 states: California, Colorado, Connecticut, Georgia, Iowa, Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah.
FIGURE 2. Cumulative rates for COVID-19–associated hospitalizations* compared with influenza-associated hospitalizations† among adolescents aged 12–17 years, by surveillance week§ — COVID-NET¶ and FluSurv-NET,** 14 states,†† 2017–2021§§
Abbreviations: COVID-NET = Coronavirus Disease 2019–Associated Hospitalization Surveillance Network; FluSurv-NET = Influenza Hospitalization Surveillance Network.
* Number of patients with laboratory-confirmed COVID-19-associated hospitalizations per 100,000 population.
† Number of patients with laboratory-confirmed influenza-associated hospitalizations per 100,000 population.
§ Surveillance week is based on the epidemiologic week for disease reporting and lasts Sundays through Saturdays. MMWR week numbering is sequential beginning with 1 and incrementing with each week to a maximum of 52 or 53. The three influenza seasons had no surveillance week 53, so values from surveillance week 52 were imputed to surveillance week 53. https://wwwn.cdc.gov/nndss/document/MMWR_week_overview.pdf
¶ COVID-NET is a population-based surveillance system of laboratory-confirmed COVID-19–associated hospitalizations in 99 counties across 14 states. COVID-19–associated hospitalizations among residents in a predefined surveillance catchment area who received a positive test for SARS-CoV-2 (the virus that causes COVID-19) during hospitalization or ≤14 days before admission are included in surveillance.
** FluSurv-NET is a population-based surveillance system of laboratory-confirmed influenza-associated hospitalizations in 81 counties across 13 states (for the period included) and is conducted annually during October 1–April 30. Influenza-associated hospitalizations among residents in a predefined surveillance catchment area who received a positive test for influenza during hospitalization or ≤14 days before admission are included in surveillance.
†† COVID-NET and FluSurv-NET sites were in the following 14 states for the period shown: California, Colorado, Connecticut, Georgia, Iowa (COVID-NET only), Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah.
§§ Cumulative COVID-19–associated hospitalization rates among adolescents aged 12–17 years during October 1, 2020–April 24, 2021, were compared with influenza-associated hospitalization rates in the same age group during October 1–April 30 across three seasons (2017–18, 2018–19, and 2019–20) using data from FluSurv-NET.
Rentahamster
Rodent Whores
No.So there were 204 hospitalization over 3 months in 14 states tracked by this service during the height of the pandemic. 204 hospitalizations. Out of millions of people in this age group, in these states. 140 or so who had underlying medical conditions as teenagers, meaning the don’t not represent the broader population of people in this age group. Again. This is not a severe risk to people in this age group.
Includes persons admitted to a hospital with between January 1, 2021 and March 31, 2021. Counties included in COVID-NET surveillance: California (Alameda, Contra Costa, and San Francisco counties); Colorado (Adams, Arapahoe, Denver, Douglas, and Jefferson counties); Connecticut (Middlesex and New Haven counties); Georgia (Clayton, Cobb, DeKalb, Douglas, Fulton, Gwinnett, Newton, and Rockdale counties); Iowa (one county represented); Maryland (Allegany, Anne Arundel, Baltimore, Baltimore City, Calvert, Caroline, Carroll, Cecil, Charles, Dorchester, Frederick, Garrett, Harford, Howard, Kent, Montgomery, Prince George’s, Queen Anne’s, St. Mary’s, Somerset, Talbot, Washington, Wicomico, and Worcester counties); Michigan (Clinton, Eaton, Genesee, Ingham, and Washtenaw counties); Minnesota (Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, and Washington counties); New Mexico (Bernalillo, Chaves, Doña Ana, Grant, Luna, San Juan, and Santa Fe counties); New York (Albany, Columbia, Genesee, Greene, Livingston, Monroe, Montgomery, Ontario, Orleans, Rensselaer, Saratoga, Schenectady, Schoharie, Wayne, and Yates counties); Ohio (Delaware, Fairfield, Franklin, Hocking, Licking, Madison, Morrow, Perry, Pickaway and Union counties); Oregon (Clackamas, Multnomah, and Washington counties); Tennessee (Cheatham, Davidson, Dickson, Robertson, Rutherford, Sumner, Williamson, and Wilson counties); and Utah (Salt Lake County).
DeepBreath87
Banned
Yes actually. Not a severe risk to children in this age group.No.
Includes persons admitted to a hospital with between January 1, 2021 and March 31, 2021. Counties included in COVID-NET surveillance: California (Alameda, Contra Costa, and San Francisco counties); Colorado (Adams, Arapahoe, Denver, Douglas, and Jefferson counties); Connecticut (Middlesex and New Haven counties); Georgia (Clayton, Cobb, DeKalb, Douglas, Fulton, Gwinnett, Newton, and Rockdale counties); Iowa (one county represented); Maryland (Allegany, Anne Arundel, Baltimore, Baltimore City, Calvert, Caroline, Carroll, Cecil, Charles, Dorchester, Frederick, Garrett, Harford, Howard, Kent, Montgomery, Prince George’s, Queen Anne’s, St. Mary’s, Somerset, Talbot, Washington, Wicomico, and Worcester counties); Michigan (Clinton, Eaton, Genesee, Ingham, and Washtenaw counties); Minnesota (Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, and Washington counties); New Mexico (Bernalillo, Chaves, Doña Ana, Grant, Luna, San Juan, and Santa Fe counties); New York (Albany, Columbia, Genesee, Greene, Livingston, Monroe, Montgomery, Ontario, Orleans, Rensselaer, Saratoga, Schenectady, Schoharie, Wayne, and Yates counties); Ohio (Delaware, Fairfield, Franklin, Hocking, Licking, Madison, Morrow, Perry, Pickaway and Union counties); Oregon (Clackamas, Multnomah, and Washington counties); Tennessee (Cheatham, Davidson, Dickson, Robertson, Rutherford, Sumner, Williamson, and Wilson counties); and Utah (Salt Lake County).
Cleared_Hot
Member
All I know is... This thing was
Bottom line is that people become so polarized that they lose site of the principles which is exactly what those in power want.
Bingo. And that's the least of it.The harms of lock downs probably don't register to you because judging by your posts, you are likely a socially inept loner who already led a "quarantine" lifestyle pre-COVID.
Bottom line is that people become so polarized that they lose site of the principles which is exactly what those in power want.
Raven117
Member
Yup. The data simply does not support that this is risk that needs to be addressed under the present circumstancesYes actually. Not a severe risk to children in this age group
Last edited:
D
Deleted member 17706
Unconfirmed Member
It says that COVID-NET, which they monitored, covers about 10% of the total US population. Very rough, obviously, but assuming it largely represents that total US population, we could multiply that number by 10, to get 2,004 adolescents out of approximately 25,000,000 (approximate number of 12 - 17 aged US population), or about 8 per 100,000. They monitored from January 1, 2021 to March 31, 2021. So about Week 1 ~ Week 12. If you look at the cumulative rates calendar below (which is supposed to be for the entire population) it was at about 18 per 100,000 population (just eyeballing it) at Week 1 2021 and 30 per 100,000 population around Week 12 or a growth of 12. Doesn't quite match up exactly, but relatively close. Also, "Number of patients with laboratory-confirmed COVID-19-associated hospitalizations per 100,000 population" in Figure 2 probably does not mean exactly the same thing as "Primary reason for admission COVID-19–related" from the first table from which the 204 number came.
Last edited by a moderator:
Rentahamster
Rodent Whores
The "No" refers to the locations. It wasn't the entirety of those 14 states. It was only select counties within those 14 states.Yes actually. Not a severe risk to children in this age group.
Hulk_Smash
Banned
That was 100% your choice.Just need to get my kids vaccinated so I can move on with my life. My sons finally started going to school and day care this week anyway. I am willing to take this small risk for their development. Being stuck at home for a year was not good for their mental health and social development. Especially in the crucial early years of their childhood.
SlimySnake
The Contrarian
No shit sherlock.That was 100% your choice.
Hulk_Smash
Banned
Oh cool so are we going from arguing about masks to arguing about variants?


D
Deleted member 17706
Unconfirmed Member
Oh cool so are we going from arguing about masks to arguing about variants?
I don't get it. Do people just want a news dump with no discussion?
Rentahamster
Rodent Whores
If you want to know the numbers for the whole country look here:So 204 12-17 year olds hospitalized over 3 months in the whole country? This is a “severe risk”? I wonder how many hospitalization there were for people in that age group falling down the steps during the same period. Maybe steps pose a severe risk too to teenagers too.
That article is a case study in framing for effect. Panic porn.
COVID Data Tracker
CDC’s home for COVID-19 data. Visualizations, graphs, and data in one easy-to-use website.
covid.cdc.gov
39,915 children in the 0-17 age range admitted to the hospital from August 1 2020 to June 6 2021.

Hulk_Smash
Banned
I don’t mind the arguing. Of course I don’t call people names and personally insult them.I don't get it. Do people just want a news dump with no discussion?
TheFarter
Banned
Great news. https://www.news-medical.net/news/2...ID-19-Findings-of-Cleveland-Clinic-study.aspx
No point vaccinating those who’ve had COVID-19: Findings of Cleveland Clinic study
more at link above.Scientists from the Cleveland Clinic, USA, have recently evaluated the effectiveness of coronavirus disease 2019 COVID-19) vaccination among individuals with or without a history of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
The study findings reveal that individuals with previous SARS-CoV-2 infection do not get additional benefits from vaccination, indicating that COVID-19 vaccines should be prioritized to individuals without prior infection. The study is currently available on the medRxiv* preprint server.
dorkimoe
Member
Like me. First dose killed me lol. Arm hurt really bad the 2nd day and then 3rd day i was on the bathroom floor but my arm stopped hurting lol. Second dose saturday for me.Your arm will likely be sore later tonight or tomorrow. But that should be it. Some people get flu like symptoms after the first shot but it is pretty rare.
BadBurger
Is 'That Pure Potato'
had 1st pfizer shot 3 hours ago.
Should I feel anything? I can't even find where they stabbed me in the arm
I got the Moderna shot myself. My arm was more sore than it typically is following my annual flu shots, and I was tired for two days. I missed my second shot appointment last week (work, always work) and just got it tonight, so I'll let you know how I feel tomorrow.
My buddy got both Pfizer shots and he had the same experience. I hope you don't suffer any side effects.
If you understand how mRNA vaccines work there is no reason to be concerned about variants
Well first, these are brand new vaccines. They've existed in theory for years, but this is the first time they've actually been put into practice, so let's not jump the gun.
The vaccines are proving to be less effective against the variants, in some cases like the B.1.351 South African variant upwards of 20% less effective at preventing infection. Good news however is that despite how effective they are at preventing infection from the variants they are something like 97% effective at preventing severe or fatal Covid-19 from any SARS-CoV-2 virus. So that's good news.
Last edited:
Raven117
Member
I was assured by science that immunity may only last 1 month, then 2 months, then 3 months, then 6 months.Great news. https://www.news-medical.net/news/2...ID-19-Findings-of-Cleveland-Clinic-study.aspx
more at link above.
BarringGaffner
Member
Funny how that works...I was assured by science that immunity may only last 1 month, then 2 months, then 3 months, then 6 months.
BadBurger
Is 'That Pure Potato'
I was assured by science that immunity may only last 1 month, then 2 months, then 3 months, then 6 months.
It's almost as if it were a process.....
Rentahamster
Rodent Whores
That's because you don't get to claim that the immunity lasts longer than 1 month, 2 months, 3 months, or 6 months, until you can actually study it for 1 month, 2 months, 3 months, or 6 months.I was assured by science that immunity may only last 1 month, then 2 months, then 3 months, then 6 months.
SF Kosmo
The Trigglypuff
It looks like some of these off-brand vaccines are not working. Russia's numbers have flattened off but they're not really low. Chile, which uses a version of SinoVac is out of control despite one of the higher vaccination rates. What a nightmare.
Brazil continues to be the world's biggest shit show, thanks to their anti-vax president and a 10% vax rate.
Canada is on track to be the most vaccinated country in the world any day now.
U.S. is not bad. We're leveling off and still behind a lot of countries, but the fact that a third of the county already got Covid and the fact that we have the best vaccines probably puts us at close to herd immunity, or at least it would if things were evenly distributed. We do still have vulnerable pockets of populations where the rate is much lower, but overall we're looking pretty good. Just stay out of Staten Island lol.
Brazil continues to be the world's biggest shit show, thanks to their anti-vax president and a 10% vax rate.
Canada is on track to be the most vaccinated country in the world any day now.
U.S. is not bad. We're leveling off and still behind a lot of countries, but the fact that a third of the county already got Covid and the fact that we have the best vaccines probably puts us at close to herd immunity, or at least it would if things were evenly distributed. We do still have vulnerable pockets of populations where the rate is much lower, but overall we're looking pretty good. Just stay out of Staten Island lol.
D
Deleted member 17706
Unconfirmed Member
Long video, but Dr. Campbell had a good talk on long term immunity and why he suspected that natural immunity would last a long time for COVID-19 just like it did for SARS and MERS.
Last edited by a moderator:
SF Kosmo
The Trigglypuff
mRNA vaccines are easy to update for variants, but I have heard they will probably move to protein subunit vaccines for boosters because they can more easily combine several variants into a single shot (probably also combined with flu as well).If you understand how mRNA vaccines work there is no reason to be concerned about variants